Last Updated on July 22, 2024
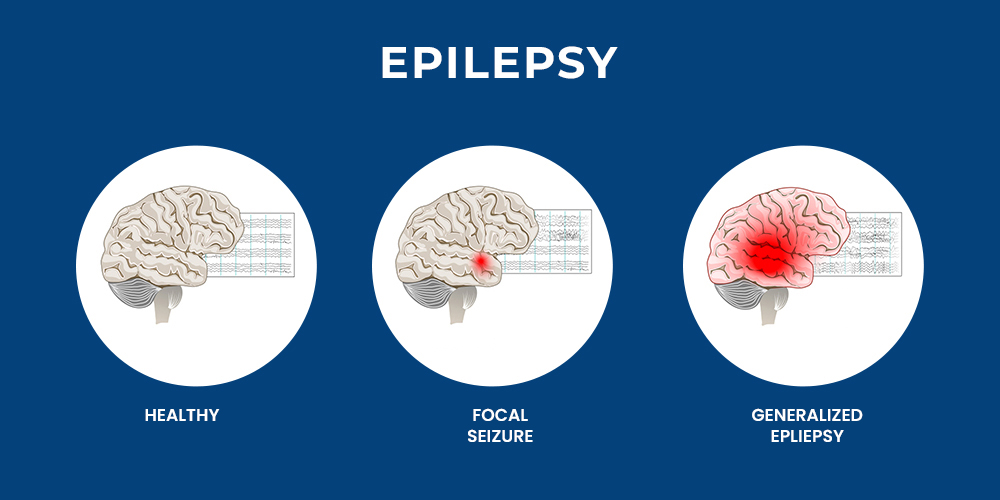
Epilepsy is a neurological condition marked by repeated seizures, which result from unusual electrical activity in the brain. Idiopathic epilepsy, a specific type of epilepsy, presents with no identifiable cause. While some potential contributors are suspected, the exact reason for its occurrence remains a mystery. It is estimated that around 1 million people in the United States are affected by this condition.
To explore more about idiopathic epilepsy, its characteristics, symptoms, potential causes, risk factors, treatment options keep on reading the blog.
What is Idiopathic Epilepsy?
Idiopathic epilepsy, also referred to as genetic idiopathic generalized epilepsy (IGE), is a group of epilepsy syndromes in which no underlying structural abnormalities in the brain are detected through imaging scans. Unlike other forms of epilepsy that may arise from brain injuries, infections, or tumors. This characteristic makes diagnosis primarily reliant on seizure types and electroencephalogram (EEG) results.
Generalized Idiopathic Epilepsy
There are several subtypes of epilepsy which are divided based on the age of onset and the predominant seizure type. These subtypes include:
- Childhood Absence Epilepsy (CAE): The age of onset of the condition is typically between 4 and 10 years. The primary seizure type is absence seizures which is characterized by brief lapses in consciousness lasting a few seconds.
- Juvenile Absence Epilepsy (JAE): The age of onset is typically between 8 and 14 years. Similar to CAE, the main seizure type is absence seizures, though they may be more frequent and prolonged.
- Juvenile Myoclonic Epilepsy (JME): This condition occurs between adolescence and young adulthood. The most common seizure type is myoclonic jerks, which are brief, involuntary muscle twitches. Individuals with JME may also experience absence seizures or generalized tonic-clonic seizures (GTCS).
- Idiopathic Generalized Epilepsy with Tonic-Clonic Seizures Alone (GTCS alone): This subtype is characterized by the presence of only GTCS, also known as grand mal seizures. These seizures involve a loss of consciousness, stiffening of the body, and jerking movements of the limbs.
It is important to note that this classification system is evolving, and some individuals may experience a combination of seizure types within the idiopathic epilepsy spectrum.
Recognizing the Signs: Symptoms of Idiopathic Epilepsy
The primary symptom of idiopathic epilepsy is recurrent seizures. The specific type of seizure will depend on the subtype of epilepsy a person has. The main types of seizure associated with this type of epilepsy are:
- Absence Seizures: These involve brief lapses in consciousness, often lasting a few seconds. The person may appear to stare blankly, or their eyelids may flutter. They typically resume activity without realizing they had a seizure.
- Myoclonic Jerks: These are sudden, brief muscle twitches that may involve the arms, legs, or face. They usually do not cause a loss of consciousness.
- Generalized Tonic-Clonic Seizures (GTCS): These are the most dramatic seizure types, characterized by a loss of consciousness, stiffening of the body, jerking movements of the limbs, and possible loss of bladder or bowel control. After the seizure, the person may experience a period of confusion and drowsiness.
In addition to seizures, some individuals with this type of epilepsy may experience other symptoms, such as:
- Learning difficulties
- Behavioral problems
- Headaches
- Dizziness
Causes and Pathophysiology
Despite the “idiopathic” (unknown cause) designation, researchers suspect a genetic predisposition plays a significant role in epilepsy. Some of the key aspects include:
- Genetic Predisposition: Mutations in genes related to ion channels, neurotransmitter receptors, and other neural pathways are believed to contribute to idiopathic epilepsy. One of the common risk factors for epilepsy is family history.
- Brain Development: Abnormalities in brain development during fetal growth may increase the likelihood of epilepsy.
- Environmental Triggers: Although the primary cause is genetic, environmental factors such as sleep deprivation, stress, and exposure to flashing lights can trigger seizures in susceptible individuals.
Preventive Strategies
Preventing idiopathic epilepsy is challenging due to its genetic nature, but certain strategies can help in managing the condition and reducing frequency of seizure:
- Genetic Counseling: For families with a history of epilepsy, genetic counseling can provide information about the risk of transmission to offspring.
- Regular Monitoring: Routine follow-ups with healthcare providers to monitor treatment efficacy and make necessary adjustments.
- Healthy Lifestyle: Adopting a balanced diet, regular exercise, and stress management techniques can support overall health and potentially reduce seizure frequency.
- Medication Adherence: Strict adherence to prescribed medication regimens is crucial in preventing seizures and maintaining seizure control.
Diagnostic Challenges and Methods
Diagnosing idiopathic epilepsy involves a detailed patient history, neurological examination, and various diagnostic tests. However, several gaps and challenges remain:
- Overlap with Other Conditions: This type of epilepsy can be mistaken for other neurological or psychiatric disorders, complicating diagnosis.
- Lack of Specific Biomarkers: There is a need for specific biomarkers to aid in the accurate diagnosis of epilepsy.
Diagnostic Methods
- Electroencephalogram (EEG): The primary diagnostic tool for epilepsy, EEG records electrical activity in the brain and can detect abnormalities present in epilepsy.
- Magnetic Resonance Imaging (MRI): While epilepsy generally shows no structural abnormalities, MRI is used to distinguish other causes of seizures, such as tumors or malformations.
- Genetic Testing: The advancement in genetic testing can help identify mutations associated with idiopathic epilepsy. This helps in diagnosis and personalized treatment.
Treatment Options
The treatment of idiopathic epilepsy aims to control seizures, minimize side effects, and improve the quality of life. Treatment options include:
- Antiepileptic Drugs (AEDs): The of epilepsy treatment include AEDs such as valproate, levetiracetam, and lamotrigine is commonly prescribed. The choice of AED depends on the type of seizures and individual patient characteristics.
- Lifestyle Modifications: Patients are advised to avoid known seizure triggers, maintain a regular sleep schedule, and manage stress.
- Dietary Therapy: The ketogenic diet, a high-fat, low-carbohydrate diet, can be effective in reducing seizures, particularly in children.
- Surgical Intervention: In cases where seizures are refractory to medication, surgical options such as vagus nerve stimulation (VNS) or resective surgery may be considered.
- Emerging Therapies: Research into new AEDs, gene therapy, and neurostimulation techniques is ongoing, offering hope for improved treatment options in the future.
Conclusion
Idiopathic epilepsy is a complex condition that requires a comprehensive approach for accurate diagnosis and effective management. By understanding its causes, recognizing early symptoms, and implementing preventive strategies, individuals can better manage this type of epilepsy and improve their quality of life. Addressing the existing gaps through research and standardization will enhance diagnostic precision and treatment efficacy, ultimately benefiting patients with epilepsy.




